“I thought I’d be better in a week. Why does my neck still hurt?”
We hear this question almost every day at CT Physical Therapy Care in Woodside.
After a car accident, you want your life back. You want to sleep without a special pillow, drive down the Grand Central Parkway without wincing when you check your blind spot, and stop relying on painkillers to finish a workday.
The truth is, whiplash is deceptive. It is not just a simple “muscle pull.” It is a complex traumatic event that damages ligaments, nerves, facet joints, and discs. Because soft tissue heals differently from a broken bone, the timeline often feels frustratingly slow if you don’t treat it correctly.
If your doctor told you to “just rest and ice it,” you might wonder why stiffness remains three weeks later.
In this guide, we break down the real recovery timeline, the medical stages of healing, the factors that might slow you down, and why New York’s “No-Fault” insurance clock makes early treatment essential.
The Short Answer: 6 to 12 Weeks (For Most People)
While every accident differs, medical research provides a reliable general timeline. Most soft-tissue injuries follow a specific biological clock.
However, “Whiplash” isn’t one-size-fits-all. In the medical world, we use the Quebec Task Force Classification to grade injury severity. Your recovery time depends heavily on your specific grade:
- Grade 1 (Mild): You feel neck pain and stiffness, but maintain a full range of motion and strength.
- Estimated Recovery: 2 to 4 weeks.
- Grade 2 (Moderate): You have neck pain AND a limited range of motion (you can’t turn your head fully). This sign implies muscle tearing.
- Estimated Recovery: 6 to 10 weeks.
- Grade 3 (Severe): You experience pain, stiffness, AND neurological signs like tingling in the arms or weakness. This nerve issue indicates nerve compression.
- Estimated Recovery: 10 to 12 weeks (or longer).
- Grade 4 (Traumatic): This involves a fracture or dislocation. This requires orthopedic intervention before Physical Therapy can begin.
The Critical Variable: Patients who start Physical Therapy within the first 7 days typically recover 40% faster than those who “wait and see” for a month.
The “Invisible Injury”: Why X-Rays Don’t Tell the Whole Story
One of the most frustrating parts of whiplash occurs when a doctor says, “Your X-rays are clean, nothing is broken.”
If nothing broke, why do you feel so much pain?
X-rays reveal only bone. They do not show the micro-tears in your muscles (strain) or ligaments (sprain). When your head whips back and forth at 4 G-forces, those soft tissues stretch beyond their limit.
Think of a severe ankle sprain. You know that a bad sprain often takes longer to heal than a clean fracture. The same logic applies to your neck. Just because the bone looks fine doesn’t mean the structure holding your head up is safe.
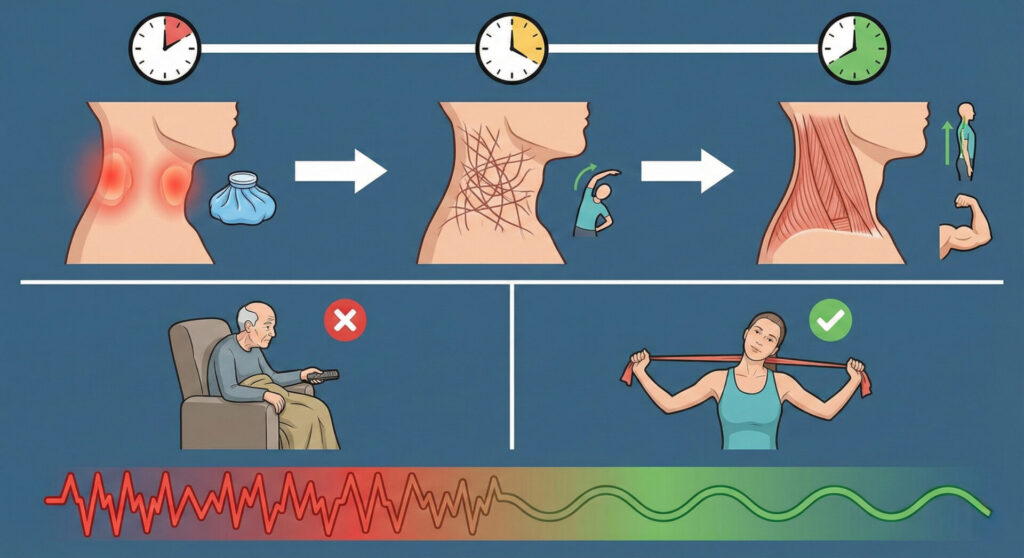
The 3 Biological Stages of Whiplash Healing
You cannot cheat biology, but you can optimize it. Your body moves through three predictable phases to repair damage. Understanding your current phase helps you manage expectations.
Phase 1: The Inflammatory Phase (Days 1–7)
- What happens: Your body enters “Crisis Mode.” Muscles lock up in a protective spasm to prevent spine movement. White blood cells rush to the area, creating swelling.
- What you feel: Severe stiffness, headaches at the base of the skull, and possibly dizziness or brain fog.
- The Goal: Reduce inflammation and pain.
- Our Approach: We use gentle manual traction to calm the spasm, along with modalities such as electrical stimulation. Do not force movement here, but do not stay in bed all day either.
Phase 2: The Repair Phase (Weeks 2–6)
- What happens: The “construction crew” arrives. Your body lays down new collagen fibers to knit torn muscles back together.
- The Danger: This new scar tissue is messy. It forms like a pile of spaghetti—disorganized and tight. If you don’t stretch it properly now, it hardens into permanent knots (fibrosis).
- What you feel: The sharp, stabbing pain dulls to a constant, deep ache. You might feel “tight” when checking your mirrors.
- The Goal: Restore range of motion. We use active stretching and joint mobilization to align new collagen fibers so they heal straight and flexible.
Phase 3: The Remodeling Phase (Weeks 6–12+)
- What happens: Your body strengthens the repaired tissue. The scar tissue matures.
- What you feel: You experience good days and bad days. You might feel fine on Tuesday, but suffer a flare-up on Wednesday after a long day at the computer. This routine becomes normal.
- The Goal: Return to full strength. We focus on posture correction (fixing “forward head”) and strengthening deep neck flexors so the pain doesn’t return next year.
5 Factors That Slow Down Your Recovery
Why does your friend heal in 3 weeks while you still hurt at 8 weeks? Several “X-Factors” influence your timeline:
- Age: As we age, discs lose hydration and ligaments lose elasticity. A 50-year-old generally takes longer to heal than a 20-year-old.
- Pre-Existing “Text Neck”: If you possessed poor posture (looking down at phones/laptops) before the crash, your neck already lacked strength. The accident acted as the “straw that broke the camel’s back.”
- Head Position During Impact: If you turned your head to the side (talking to a passenger) at the moment of impact, the injury often proves more severe than if you looked straight ahead.
- Stress and Anxiety: High stress levels increase muscle tension. If you feel anxious about driving or dealing with insurance, your shoulders tighten, slowing down recovery.
- Delayed Treatment: This factor matters most. Waiting 4 weeks to seek help allows scar tissue to set incorrectly. Breaking down old, hard scar tissue takes much longer than molding fresh tissue.
The “Insurance Timeline”: A New York Reality Check
You face a second timeline: The Insurance Clock.
As we explained in our article on NY No-Fault Insurance, you possess coverage for “necessary” medical treatment. However, insurance companies operate as businesses. They look for reasons to stop payments.
The “Gap in Care” Trap
If you visit the ER on Day 1, but then wait 3 weeks to start Physical Therapy, the insurance adjuster will flag your file. They will argue: “If they really hurt, they wouldn’t have waited 3 weeks.”
This gap can cause a denial of treatment, leaving you with the bill and the pain.
Maximum Medical Improvement (MMI)
Insurance companies often use this term. It essentially means “you are as good as you’re going to get.” Around the 12-week mark, independent doctors may review your file. If you show no consistent attendance or improvement, they may cut off benefits.
Consistency matters. Regular attendance at Physical Therapy proves to the insurance company that you remain injured and actively work to recover.
Why “Rest and Wait” Fails
Decades ago, doctors prescribed a “soft collar” and bed rest for whiplash. We now know this damages recovery.
Immobilizing a neck for too long causes muscle atrophy (weakness) and stiffness. The modern approach requires “Active Recovery.”
- Passive Recovery (Avoid this): Relying on painkillers, heating pads, and waiting. This masks pain but lets muscles heal tightly.
- Active Recovery (Do this): Gentle guided movement, nerve glides, and strengthening. This technique teaches the body how to heal.
When Does “Acute” Become “Chronic”?
If you pass the 3-month mark and still feel significant pain, you may have entered the Chronic Phase.
This condition doesn’t mean you remain broken forever. It usually means:
- Hidden Pathology: We may need to look for a specific disc herniation or facet joint injury that requires different treatment.
- Sensitization: Your nervous system stays on “high alert” and interprets normal movement as pain.
- Compensation: You changed the way you move (guarding) to avoid pain, which now causes new pain in your shoulders or upper back.
At CT Physical Therapy Care, we specialize in chronic cases. We treat posture, mechanics, and nerves to break the cycle of chronic pain.
Don’t Settle for “Living With It”
You can’t rush healing, but you can stop delaying it.
If you live in Woodside, Maspeth, Sunnyside, or Jackson Heights, you don’t have to navigate this timeline alone. We can help you determine if you are in Phase 1 or Phase 3, and give you the exact roadmap to get out of pain.
Your Recovery Checklist:
- Don’t Wait: The window for optimal healing is now.
- Stay Consistent: Don’t skip appointments.
- Trust the Process: Healing acts as a marathon, not a sprint.
Contact CT Physical Therapy Care today to schedule your evaluation. Let’s get you back to 100%—not just “good enough.”
Frequently Asked Questions (FAQ)
Can I drive with whiplash? It depends on your range of motion. If you cannot turn your head to check your blind spot without severe pain, you cannot drive safely. Furthermore, driving often increases stress on neck muscles. We recommend resting from driving for the first few days if possible.
Why is my pain worse in the morning? Inflammation tends to pool when we stay still. When you sleep, your joints stiffen up. This mechanism explains why the first 30 minutes of the morning often feel the most painful. A warm shower and gentle range-of-motion exercises can help loosen things up.
Will a heating pad help my whiplash? In the first 48-72 hours (Phase 1), we generally recommend Ice to reduce inflammation. After the first 3 days, Heat works excellently for relaxing tight muscles and increasing blood flow to the area.
How long does dizziness last after whiplash? Dizziness usually fades within the first 2-3 weeks. If you still feel dizzy after that, or if the room spins when you roll over in bed, you may have a vestibular issue or a concussion. Please read our guide on Dizziness here.
